WORLDWIDE
-
Prospect
- 20190129 (National University of Taiwan and the Ministry of Obstetrics and Gynecology Reproductive Medicine Center) land lease briefing
- 181012 (Taiwan University) (University) Briefing c (B2 6F Case A Projection)
- Briefing on the lease of land for the Reproductive Medicine Center of the University of Taiwan
- Introduction to Athens Design

Medical appointment
Home > Medical appointment > Appointment area > Within the clinic
Within the clinic
Pelvic examination, also known as internal medicine, is the most basic physical examination of obstetrics and gynaecology. The predecessor of obstetrics and gynecology is always a young doctor who can't forget this book (internal diagnosis). Young gynaecologists often Use the diagnosis to judge whether to open a prescription or directly jump into a supersonic wave... and other advanced equipment inspections, health insurance review has an unwritten rule: no internal diagnosis records, can not declare gynecological ultrasound. The following describes pelvic examination. (This page References and excerpts from Novack's Gynecoloy 13rd Ed. Section I. Principles of Practice)

| Pelvic examination | The most common typical posture is the Dorsal lithotomy position. It is best to empty the urine first. | The patient's foot should be placed comfortably on the edge of the hip on the tripod. The genital part of the lower edge of the examination table can be completely inspected. The voyeur (duck mouth) can be placed into the vagina without hindrance. |

| Visual examination (Inspection) | Vulva vulva, perineum Perineum (and lower abdomen, pubic humerus, anus, buttocks and caudal vertebrae) should be carefully examined for ulceration or suppuration to consider bacterial culture | Pay attention to any lesions, red, swollen, pigmented, hard or abnormal skin texture, trauma, scraping, silt... |
| palpation (Palpation) | Pathological section | Any lesion should be measured in size and carefully describe the appearance and palpation feeling (movable, tender, hardness...) |
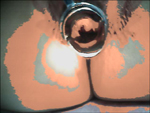
| Peeping device (Speculum) (duck mouth) | Put into the vagina, carefully check the cervix, especially in the vagina area, pay attention to the vaginal dome, often have lesions (such as cauliflower) Consider doing a Pap smear or considering endometrial sampling ulceration or suppuration. Consider any obvious lesions in bacterial culture. Consider pathological sectioning. | The duckbill should be lubricated and warmed before putting it in. It is best to say it orally. Otherwise, some people will be shocked. The length of the duckbill should be appropriate. It is necessary to see the cervical cervix position factor before and after the head is tilted. It can be expanded and moved first. Duckbill opening, find it and then rotate it to the appropriate size. At the end of this stage, gently unscrew and take out the duckbill. |
| palpation (Palpation) | The index finger and middle finger gently enter the vagina, carefully palpate the vagina, vaginal dome and cervix to see if there is any hard block or abnormality. | Can be lubricated first, the vagina is actually similar to the H type, the corner is easy to ignore |
| Check with both hands (Bimanual) | Then the finger enters the posterior iliac and touches the uterus to see if there is any pain and the other hand touches the upper part of the pubis. The uterus can be completely touched and then gently touched on both sides of the appendage Adnexa, pay attention to any painful swelling. | Uterine inflammation will increase the pain at this time to pay attention to the size, shape, degree of freedom, appearance, hardness and position of the uterus (forward leaning backward or middle) Carefully record size, shape, degree of freedom, shape, hardness and structure |
| Anal diagnosis (Rectal exam) | Pay attention to the quality of the sphincter, pelvic relaxation, hemorrhoids, anal and rectal lesions. | 40 years old or older recommended regular anal diagnosis |
| Vaginal anal examination (Rectovaginal) | Vaginal and anal examination can more clearly understand the extent of the lesion | Help with cervical cancer staging or rectal anal cancer staging |
After the pelvic examination (internal diagnosis) is completed, the patient should be informed of any findings. If you are normal, please feel relieved. If there is any abnormality, immediately inform the patient with a clear and concise statement and discuss the next step and recommended examination or treatment. Physicians must provide the latest information on the obstetrics and gynaecology of patients. Physicians need to work hard from formal medical education, trainee internships, personal experiences, teachers, textbooks, on-the-job education, new knowledge speeches, written or online professional journals. Get the latest knowledge to serve patients. Today's medical insurance payments cannot keep up with medical advances, and physicians should not provide up-to-date medical information because insurance is not paid.

